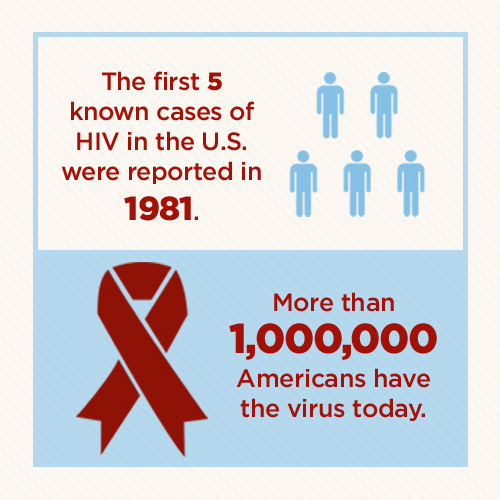
The U.S. Centers for Disease Control (CDC) reported the first five known cases of HIV in Los Angeles in June of 1981. The previously healthy gay men had contracted pneumonia and two died. Today, more than a million Americans have the virus.
Being diagnosed with HIV was once a death sentence. Now, a 20-year-old man with HIV who begins treatment early can expect to live to 77 — the average lifespan of an average American man. The disease, which attacks the immune system, can be controlled by modern-day antiretroviral medications.
Prevalence, Incidence, and Death Rates: Then and Now
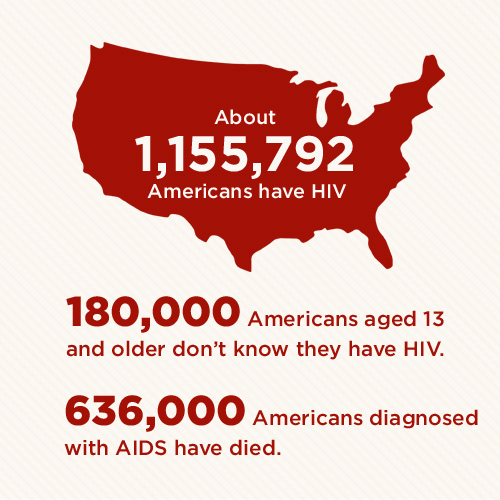
An estimated 1,155,792 Americans have HIV. About 180,900 people aged 13 and older don’t know they have it.
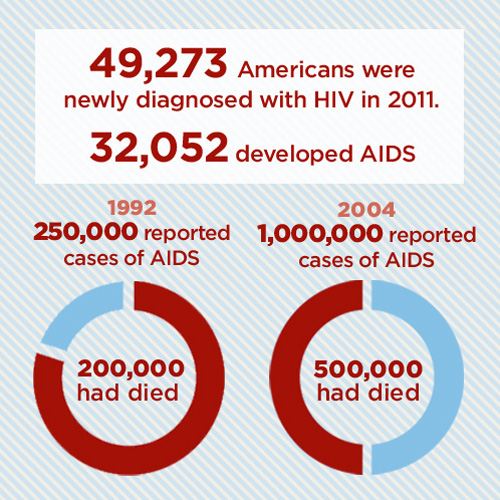
An estimated 49,273 Americans were newly diagnosed with HIV in 2011, but only 32,052 developed AIDS. This is in striking contrast to the early days of HIV/AIDS.
According to the American Federation of AIDS Research, of the 250,000 cases of reported AIDS cases, 200,000 already had died by 1992. By 2004, a million cases had been reported and 500,000 had died.
In 2010, 15,529 people accounted for 2 percent of total AIDS deaths in the U.S. So far, 636,000 people in the U.S. diagnosed with AIDS have died.
Demographics: Who Gets HIV and How?
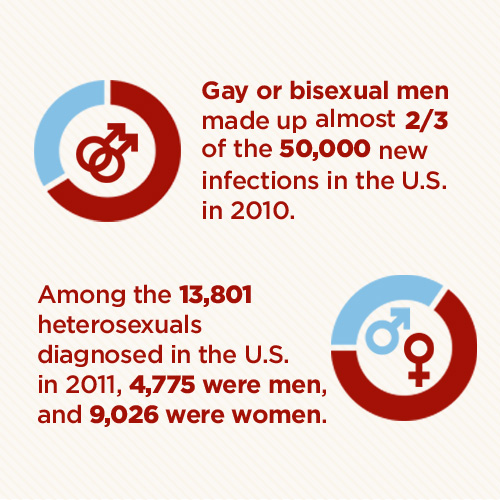
According to the CDC, gay or bisexual men made up almost two-thirds of the 50,000 new infections in the U.S. in 2010. In 2011, 30,896 infections in the U.S. came as the result of male-to-male sexual contact. While gay men continue to represent most HIV infections in the U.S., anyone who practices unsafe sex or shares IVs can contract HIV. Among the 13,801 heterosexuals diagnosed in the U.S. in 2011, 4,775 men and 9,026 women contracted the virus.
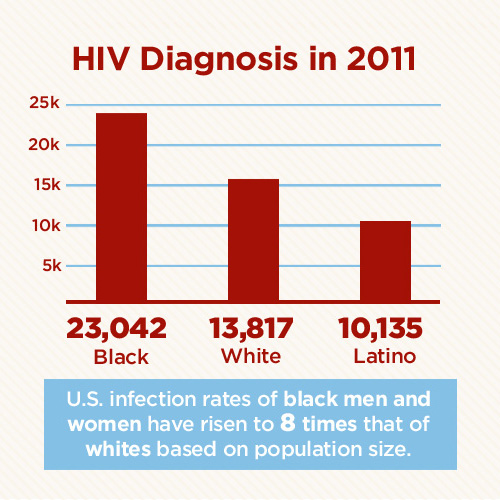
When it comes to race, 23,042 of those diagnosed in the U.S. in 2011 were black, 13,817 were white, and 10,135 were Latino. Infection rates in the U.S. of black men and women have risen to eight times that of whites based on population size.
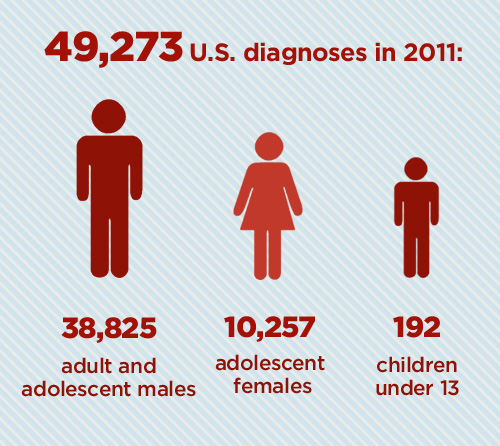
Of 49,273 diagnoses in the U.S. in 2011:
- 38,825 were adult and adolescent males
- 10,257 were adolescent females
- 192 were children under age 13
Location: A Big Problem Worldwide
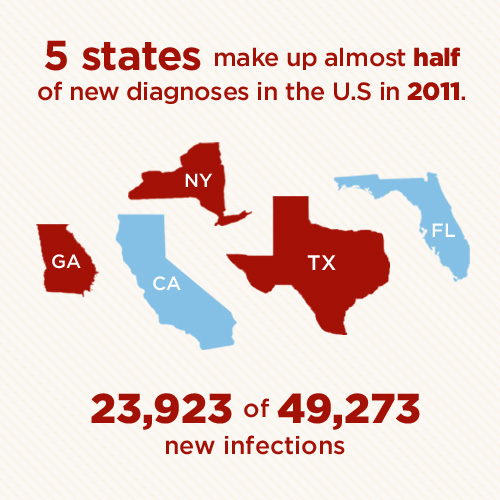

Five states alone make up almost half of new diagnoses in the U.S. in 2011. These five states account for 23,923 of 49,273 new infections, according to the CDC:
- California
- Florida
- Texas
- New York
- Georgia
Number of infections on other continents:
- Asia: 4.7 million
- Latin America: 2 million
- Eastern Europe and Central Asia: 1.5 million
Prevention: Protect Yourself and Your Loved Ones
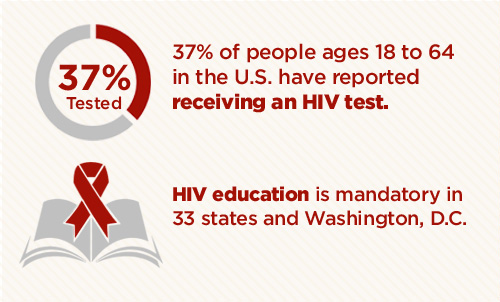
It’s important for people — especially high-risk groups — to be tested frequently. Starting HIV treatment early is important for best outcomes. Approximately 37 percent of people ages 18 to 64 in the U.S. have reported receiving an HIV test. HIV education is mandatory in 33 states and in Washington, D.C.
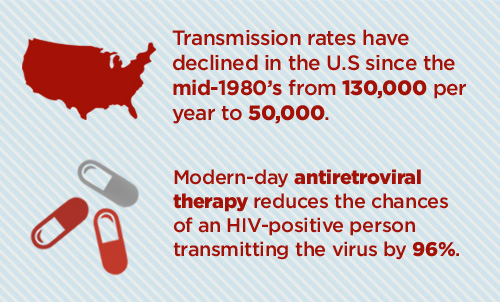
Preventing transmission of HIV is as important as treating those who have it, from a public health perspective. There has been remarkable progress in that regard. For example, modern-day antiretroviral therapy can reduce the chances of an HIV-positive person transmitting the virus by 96 percent.
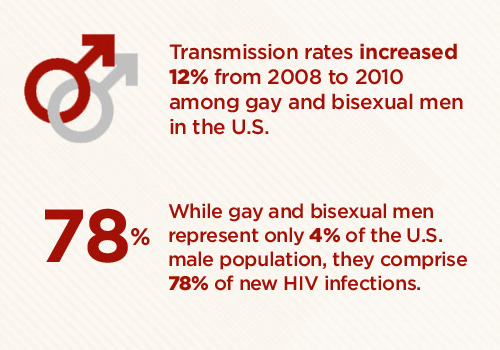
There has been a sharp decline in transmission rates in the U.S. since the mid-1980s: from 130,000 per year to 50,000. However, transmission rates increased 12 percent from 2008 to 2010 among gay and bisexual men, who comprise the U.S. population most at risk. While gay and bisexual men represent only 4 percent of the male population in the U.S., they comprise 78 percent of new HIV infections.
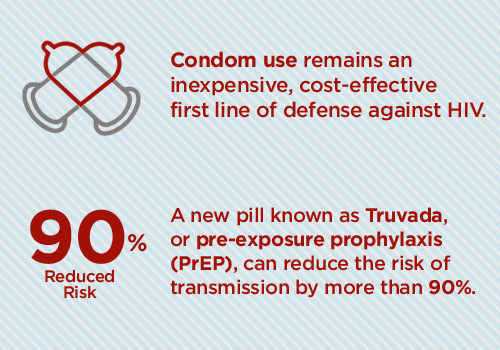
Condom use remains an inexpensive, cost-effective first line of defense against HIV. A new pill known as Truvada, or pre-exposure prophylaxis (PrEP), also offers protection. An HIV-negative person can protect themselves from contracting HIV by taking a once-a-day pill. When taken properly, PrEP can reduce the risk of transmission by more than 90 percent.
Cost of HIV/AIDS
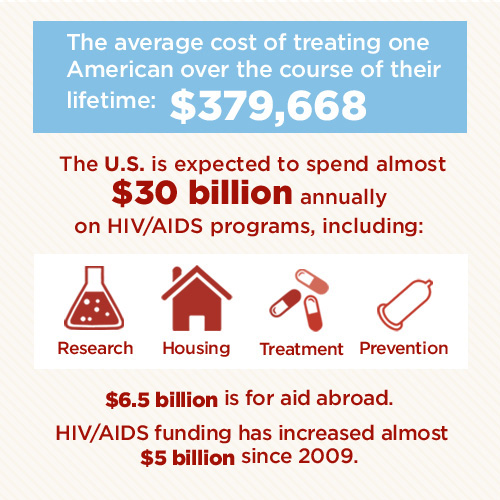
There is still no cure for HIV, and it can take a huge financial toll on those living with it. The U.S. is expected to spend almost $30 billion annually on HIV/AIDS programs, including:
- research
- housing
- treatment
- prevention
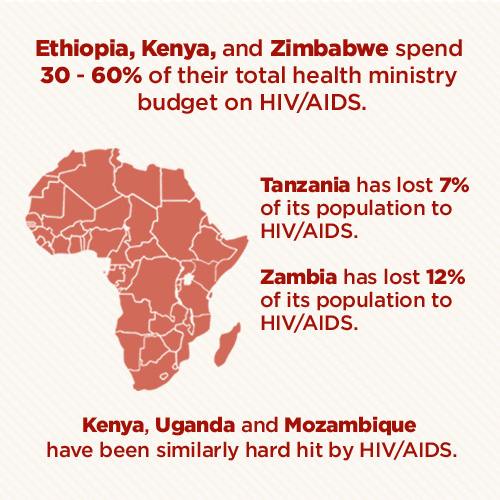
Not only are life-saving medications expensive, but massive numbers of people in hard-hit countries with limited resources have died or are unable to work due to HIV/AIDS. This has affected these nations’ development.
Unlike diseases that affect children or the elderly, HIV hits people during their working years. Countries end up with lost productivity and, in many cases, a significant reduction in the workforce. This all adds up to severe impacts on these national economies.
According to the U.S. Census Bureau, Zambia has “lost” more than 1.6 million people to HIV/AIDS — almost 12 percent of its population. Tanzania is “missing” more than 3.2 million people to HIV/AIDS — 7 percent of its population. Kenya, Uganda, and Mozambique have been similarly hard hit.
Some African countries such as Ethiopia, Kenya, and Zimbabwe spend between an estimated 30 and 60 percent of their total health ministry budget on HIV/AIDS.
The average cost of treating a person with HIV over the course of their lifetime is $379,668. The CDC reports that prevention interventions are deemed cost effective if they prevent an infection in one person for less than that.
Article Sources:
- Cohen, M.S., Chen, Y.Q., McCauley, M., et al. (2011, August 11). Prevention of HIV-1 Infection with Early Antiretroviral Therapy. The New England Journal of Medicine, 365, 493-505. Retrieved from http://www.nejm.org/doi/full/10.1056/NEJMoa1105243#t=articleTop
- Economic implications of HIV/AIDS: A crisis in development. (2011, June 25). The UC Atlas of Global Inequality. Retrieved from http://ucatlas.ucsc.edu/health/aids/econ_imp.php
- Global statistics. (2012, June 6). AIDS.gov. Retrieved from http://www.aids.gov/hiv-aids-basics/hiv-aids-101/global-statistics/
