According to a group of Swedish researchers, based at Lund University, a highly virulent strain of HIV is capable of causing acquired immunodeficiency syndrome (AIDS) within just five years. The strain in question, labeled A3/02, was first discovered in 2011 and is considered part of a worrying rise in the number of cases of infection caused by “recombinant” forms of the deadly virus.
Human immunodeficiency virus (HIV) can be divided into two separate types, including HIV type 1 (HIV-1) and HIV type 2 (HIV-2). HIV-1 is the most typical, pathogenic strain of the virus, which can be further broken down into additional subtypes and circulating recombinant forms (CRF).
All in all, there are more than 60 epidemic strains of HIV-1, responsible for infecting people all over the globe. Typically, a specific geographic region is dominated by just one or two of these strains. If an individual becomes infected with two different strains of HIV-1, however, a recombination form of the virus can occur. The significance of this was briefly touched upon by doctoral student Angelica Palm, who studies at Lund University:
“Recombinants seem to be more vigorous and more aggressive than the strains from which they developed.”
The impact of these subtypes and CRFs on disease progression still remains poorly understood. This is where the Swedish researchers sought to delve a little deeper, by assessing the impact that the new CRF strain has on HIV-infected patients.
The Study
The researchers established the subtype/CRF of over 150 HIV-infected participants, hailing from the Republic of Guinea-Bissau – a country situated on the coast of West Africa, and bordered by Senegal and Guinea.
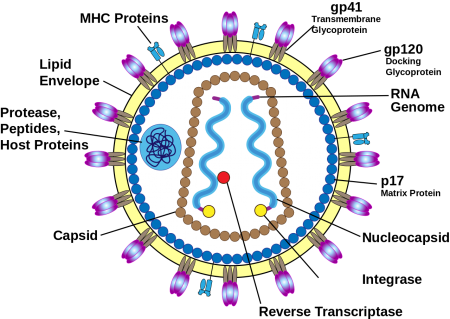
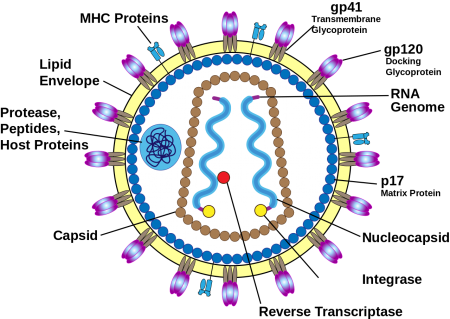
Structure of HIV virus, including the envelope glycoproteins, gp120 and gp41.
The scientists explored a specific region of one of the HIV virus’ genes, called env, which codes for the surface protein gp160. Ultimately, this protein is then broken down by an enzyme to produce two other functionally essential structures, gp120 and gp41. This helped with identification of the specific subtype/CRF for each subject.
The major subtypes discovered from the participants were called CRF02_AG and A3, affecting 53 percent and 29 percent of people, respectively. Interestingly, 13 percent of all subjects tested positive for A3/02, a recombinant form that stems from CRF02_AG and A3.
CRF02_AG and A3 were certainly anticipated, as they are the most common strains of HIV found in Guinea-Bissau. However, the A3/02 recombinant represented a relatively new strain, whose virulence was yet to be truly tested.
Once the HIV strain had been determined, the researchers wanted to identify how particular subtypes and CRFs influenced disease progression. As a consequence, they calculated a series of hazard ratios (HRs), adjusting for age and gender at seroconversion – the point at which the subjects first tested positive for HIV antibodies. The HR values provide an indication of the risk of developing AIDS, as they took into account the time from estimated seroconversion to developing AIDS and AIDS-related death.
HIV A3/02 Recominant Strain Highly Virulent
The researchers established that participants who were infected with the new, highly virulent form of HIV (A3/02) demonstrated an average three-fold increased risk of AIDS and AIDS-related deaths, compared to those people infected with the A3 strain.
People infected with the recombinant A3/02 strain also developed AIDS much quicker. For A3/02 sufferers, the estimated time from seroconversion to AIDS was five years, whereas the estimated time from seroconversion to death was just eight years.
People infected with CRF02_AG and A3, meanwhile, seemed to show slower disease progression and survived a number of years longer, as evidenced:
- CRF02_AG: seroconversion to AIDS was 6.2 years
- CRF02_AG: seroconversion to death was nine years
- A3: seroconversion to AIDS was 7.2 years
- A3: seroconversion to death was 11.3 years
Thus far, this strain of HIV has only been observed in populations of West Africa. Meanwhile, a number of other studies seem to show that recombinant strains of HIV are beginning to gain a foothold across the globe. According to a recent press release, the university suggests this problem is particularly pertinent to the United States and many countries in the European Union, where immigration levels are typically high.
As a consequence, the authors describe the development of a “complex HIV flora,” the likes of which were not evident during the preliminary stages of the epidemic, where only a sparse few non-recombinant viruses were responsible for infection.
The Future
Patrik Medstrand, a Professor of Clinical Virology at Lund University, ruminated over the implications of these new recombinant forms of HIV and the scientific community’s need to study them:
“HIV is an extremely dynamic and variable virus. New subtypes and recombinant forms of HIV-1 have been introduced to our part of the world, and it is highly likely that there are a large number of circulating recombinants of which we know little or nothing. We therefore need to be aware of how the HIV-1 epidemic changes over time.”
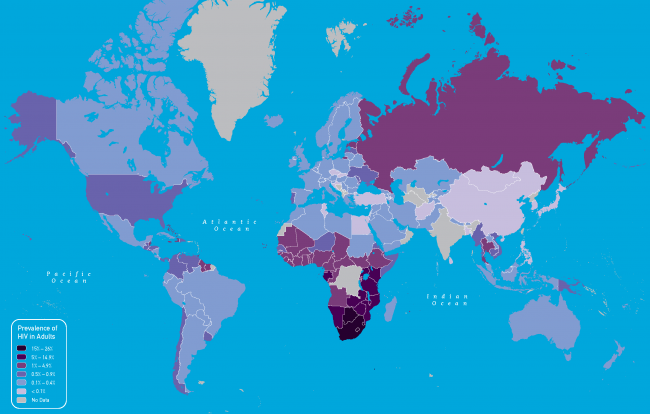
Currently over 35 million people are living with HIV across the globe, with over 35 million deaths having been recorded since AIDS first emerged, during the 1980s.
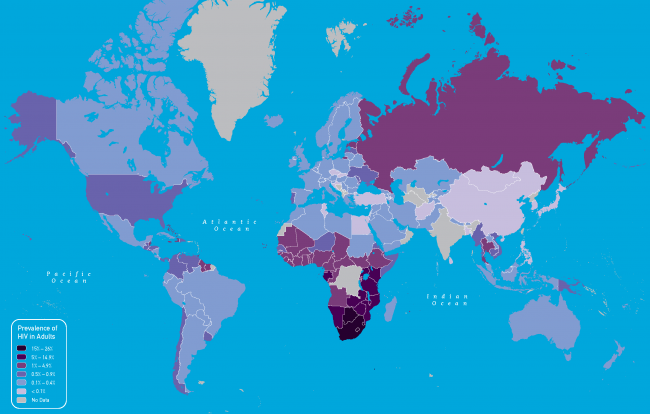
Worldwide prevalence of HIV in adults for 2011 (Image credit: Centers for Disease Control and Prevention)
Palm and her colleagues aim to continue research into the characteristics of different strains of recombinant HIV, and their presence in carriers throughout Europe. The study could also be useful for health authorities, with strain-specific knowledge potentially proving useful for future treatment strategies.
The recent findings were published in the latest issue of the Journal of Infectious Diseases, entitled Faster Progression to AIDS and AIDS-Related Death Among Seroincident Individuals Infected With Recombinant HIV-1 A3/CRF02_AG Compared With Sub-subtype A3.
By James Fenner

 What is HIV?
What is HIV?%20web.jpg)

